The nose is a central anatomic feature of a person’s identity and self-image. The nasal appearance can also positively or negatively affect self-confidence. When communicating face-to-face, the nose is central to the field of vision and will always be seen during the subconscious facial scan that occurs at that time.
Self-awareness of the appearance of nasal aesthetics has existed for many centuries, but until modern times, little was possible to predictably and accurately change the appearance of the nose—materials engineering and machining had not advanced enough to allow construction of delicate and exact surgical instruments required to perform the procedure with precision. In addition, there was no safe and adequate manner in which to provide anesthesia for nasal surgery.
Fortunately, advancements in all these areas—as well as an enormous amount of plastic surgery research—have made possible the modern-day nose surgery (rhinoplasty), which is very predictable and safe. In fact, a multitude of surgical techniques and surgical planning methods exist now that were yet to be described even just a few years ago. The combination of these factors has made the modern rhinoplasty a highly sought-after plastic surgery procedure—one that can yield exceptional results
“Dr. Herring and his staff exceeded my expectations. My self confidence/esteem has increased after my surgery. Everyone is informative and answers all questions and makes sure you understand thoroughly. Pre-op, operation, and post-op is all thorough. Safety and health are a priority of the staff.”
Procedure at a Glance
- Procedure
- Reshape the nose by reducing or increasing the size, removing a hump, changing the shape of the tip or bridge, narrowing the span of the nostrils, or altering the angle between the nose and upper lip; correct impaired nasal breathing caused by natural and/or trauma-related structural abnormalities (sometimes covered by insurance)
- Length
- About 1–2 hours, sometimes longer
- Anesthesia
- IV sedation with local anesthesia, or general anesthesia
- In/Outpatient
- Usually outpatient
- Side Effects
- Temporary swelling and stiffness, bruising around the eyes and nose, headaches, and possible bleeding
- Recovery
- Back to non-strenuous work: 1–2 weeks; more strenuous activities: 2–3 weeks; avoid sunburn and contact to the nose: 8 weeks; final appearance: 1 year or more
- Duration of Results
- Permanent
- What Is Rhinoplasty?
- Reasons for Rhinoplasty
- Surgical Techniques & Maneuvers for Rhinoplasty
- Nasal Anatomy & Appearance
- Open vs. Closed Rhinoplasty
- Consultation & Preoperative Planning
- Rhinoplasty Procedure
- Rhinoplasty Recovery
- Cost of Rhinoplasty
- Additional Rhinoplasty FAQs
What Is Rhinoplasty?
Rhinoplasty is a procedure that changes the size and/or shape of the nose by modifying internal nasal structures. In general terms, the appearance of the nose is determined by the underlying anatomy that supports the nasal skin, and this internal framework (consisting of cartilage and bone) can be altered to modify various nasal characteristics—ultimately enhancing the aesthetic of the nose. If indicated, the internal structures of the nose can also be modified to address congenital and/or trauma-related issues, allowing for improved nasal breathing.
Goals of Rhinoplasty*
- Increase or decrease the overall size and/or width of the nose
- Reduce a hump/bump on top of the nose
- Raise or lower the nasal bridge
- Decrease an overly wide nasal tip (bulbous tip)
- Improve the symmetry of the nasal tip and/or nostrils
- Straighten a crooked nose
- Increase or decrease the projection of the nasal tip
- Modify the angle between the nose and upper lip
- Reduce wide or flaring nostrils
- Correct a deviated septum and/or other structural issues
*Individual goals may vary
At our practice, board-certified plastic surgeon Stephen Herring, MD has helped numerous women and men achieve exceptional nasal form and function via rhinoplasty. In changing the shape of the nose, his aim is always to retain or create normal anatomy in relation to the face while also preserving (or even enhancing) a patient’s ability to breathe optimally through the nose. Dr. Herring is very familiar with anatomical nasal characteristics that are desirable or considered “normal” for a variety of different ethnicities, and he is able to customize treatment to meet the specific needs and aesthetic preferences of each individual.
If you are considering rhinoplasty, please contact us today to book a consultation and discover how Dr. Herring can address your particular concerns to achieve the nasal look and/or function you desire.
What Are Some Common Reasons Patients Seek Rhinoplasty?
There are a multitude of specific reasons patients seek a rhinoplasty. Unusual or disproportionate nasal anatomy can cause loss of self-confidence and self-assurance. Lack of self-confidence for any reason can be self-defeating, potentially affecting every aspect of a person’s life. Rhinoplasty can and has improved self-confidence and self-assurance levels in many patients.
The most common reason patients seek rhinoplasty is a prominent nasal dorsum, which some patients refer to as a nasal “hump.” This can occur as a result of trauma, which is quite common, or can result from a familial (genetic) trait. A dorsal “hump” is generally, but not always, considered more masculine. Patients, especially women, will frequently state at the consultation, “I hate the way I look from the side.” They will also convey that they are very self-conscious about this trait, especially when observed in a profile-view photograph. Patients will also frequently state, “I have always hated my nose, and I finally decided to do something about it.”
In general, the aesthetically preferred nasal dorsum for men is straight or slightly over-contoured. For women, the aesthetically preferred nasal dorsum is typically straight or slightly under-contoured. Of course, there are always some exceptions to these considerations. Bob Hope, the famous comedian, often self-deprecating, joked about his “ski slope nose,” which was very feminine. As a result, his nose became a significant part of his public image to the degree that it was frequently a focus of his caricature. This emphasizes the enormous impact nasal aesthetics have on a person’s overall image. While his nose was feminine, he also had many feminine facial features, so his nose “fit” his general appearance. This emphasizes the importance of proportion and congruence in relation to the concept of beauty. While many patients have never thought about the objective criteria of beauty and proportion, they all understand the general concept.
Another common concern patients voice, and therefore another reason for seeking rhinoplasty, is related to the nasal tip. Nasal tip problems are widely varied. The great variation in nasal tip anatomy combined with the wide variation in facial structures means there are many different solutions (surgical maneuvers) to correct these problems. A frequent concern voiced by patients is the broad nasal tip. Patients might state, “My nose is too big,” and they mean that the nasal tip is too broad. This nasal tip problem is also referred to as a “boxy nasal tip.” Patients with a “boxy tip” have a squared-off appearance to the nasal tip rather than a more pointed tip. This group of patients may also have an “over-projecting tip,” which means the nasal tip is too long.
Another common complaint patients seeking rhinoplasty voice is the drooping nasal tip. This is typically a familial trait that is expressed to varying degrees, and is usually a result of overgrowth of the nasal septum and alar (lower lateral cartilages). The “drooping tip” can also be a result of an undergrowth of the structures (nasal septum and anterior maxillary spine) at the junction of the upper tip and nose. In this circumstance, the nasal tip is really not drooping, it just appears to be drooping because of the under-contouring of the aforementioned area.
Asymmetry of the nasal tip is another concern patients voice when seeking rhinoplasty. Asymmetry can occur in the tip of the nose, and also in the dorsum of the nose (see section below), or both. Many patients with nasal asymmetry will report a history of trauma, and this is especially true for the nasal dorsum. Nasal trauma can also result in airway obstruction, which can also be addressed at the same time as the aesthetic rhinoplasty.
Patients often seek rhinoplasty for asymmetry (deviation) of the nasal dorsum, simply stating, “My nose is crooked.” This problem may be developmental, but patients frequently report that nasal trauma was the cause of the dorsum asymmetry. A commonly observed clinical situation is the patient that suffers nasal trauma and does not seek immediate care. The nasal trauma results in a shifting of the nasal dorsum (asymmetry), but the acute swelling masks the deviation. Later, when the swelling subsides, the asymmetry of the nasal tip becomes very obvious, and by this time, the nasal structures have healed in this abnormal position. The dorsum asymmetry can be severe or slight, and the severity of the deviation in part determines the technique(s) that are chosen to correct the problem. In some circumstances, the dorsal nasal structures are simply shifted to the midline, and in other circumstances, a graft is used to correct the problem. The primary structures that are involved in the correction of the deviated septum are the cartilaginous septum and the nasal bones, which—in addition to undesirable aesthetics—can cause obstruction of breathing.
A less common concern patients voice is the width of the nose (base of nose too wide). In this group of patients, the alar cartilages flare too widely, changing the shape of the nostrils and the appearance from a front view. When planning to address this concern, many factors—including facial shape, gender, habitus, ethnicity, and most importantly, the patient’s goals—should be considered. In some circumstances, and depending upon the specific technique that is chosen, this concern is addressed at a later time (staged surgery) due to the potential problems with blood supply.
In summary, there are many reasons patients seek the rhinoplasty procedure. The majority of patients have more than one anatomical trait that can be corrected. It is important for patients pursuing rhinoplasty to understand that a new nose is not created (except in the circumstance of reconstruction), but rather their own nose is changed to a more ideal shape. It is also important to realize that the ideal nasal shape for one person may not be the ideal shape for another person, including family members. Most every plastic surgery procedure has limitations. It is important for the patient seeking rhinoplasty to understand those limitations before making the decision to have surgery.
Understanding Nasal Anatomy & Its Effect on Nasal Appearance
Nasal anatomy is so important that it can affect an individual’s entire image. As a result, the plastic surgeon should always consider the patient’s image when discussing the rhinoplasty procedure. A plastic surgeon’s detailed knowledge of normal nasal anatomy is a critical factor for the successful rhinoplasty. It is also very important for the plastic surgeon to understand normal anatomic variation, how this relates to the appearance of the nose, and how the nasal shape relates to the facial structures and the patient’s image—meaning self-image and the patient’s image to the public. In addition to the anatomy of the nose, it is also important for the plastic surgeon to understand the physiology (function) of the nose and how this relates to the anatomy.
When planning a rhinoplasty, the surgeon should consider facial shape, the gender of the patient, the ethnicity of the patient, and most importantly, the patient’s goals. Many (but not all) rhinoplasty procedures result in very subtle changes. Even the most subtle changes in nasal aesthetics can make an enormous difference in the general appearance. An example of this phenomenon is the well known actress Jennifer Grey. In her Dirty Dancing years, she was pre-rhinoplasty and was very attractive. Sometime after that movie was filmed, she underwent a rhinoplasty. While the changes in her rhinoplasty were subtle and very appropriate, she now has a completely different appearance. The rhinoplasty procedure that changed a small part of her anatomy completely altered her appearance and image. She was attractive before rhinoplasty, and is attractive after rhinoplasty, but is very different.
The major structures of the nose include the nasal bones, the nasal septum, the lower lateral cartilages (alar cartilages), and the upper lateral cartilages. There are many other anatomical entities that have been described in addition to the aforementioned that can be addressed at the time of rhinoplasty. The nasal septum is the main support of the nose. It is in the midline of the nose and consists of cartilage and bone. The nasal septum is composed of bone in (approximately) the upper one half, and cartilage in (approximately) the lower one half. If this structure is damaged or is missing, the result is a depressed dorsum that is sometimes called a “saddle nose.” This requires a reconstructive rhinoplasty procedure to repair. Both of the components of the septum are frequently altered during the rhinoplasty procedure. Overgrowth of the nasal septum can result in many anatomic variations, including a drooping nasal tip, the over-projecting nose, and the nasal “hump.” Of course, all of these conditions can exist at the same time.
The lower lateral (alar) cartilages give the nasal tip its shape. They also serve a physiological purpose in keeping the nares open during inspiration. There are enormous variations in the shape of the lower lateral cartilages, which give enormous variation in the shapes of the tip of the nose. The lower lateral cartilages cause the broad (“boxy”) nasal tip, the drooping nasal tip, and the over-projecting nasal tip. The alar cartilages are almost always altered to some degree during the rhinoplasty procedure.
In some circumstances, the anatomy of the lower lateral cartilages can be quite striking and overpower the other features of the face. Karl Malden represents an example of the classic “broad nasal tip.” This appearance is caused by the overgrowth and broadening of the alar cartilages. The actor Jimmy Durante is another classic example of the nose overpowering the face. In his case, there was overgrowth of the lower lateral cartilages and the nasal septum. So dramatic was the nasal anatomy of these actors that it became their trademark.
The upper lateral cartilages of the nose serve an aesthetic and physiological purpose. The upper lateral cartilages of the nose support the middle vault and prevent a “pinched” appearance, which can occur if these cartilages are damaged or are underdeveloped. The upper lateral cartilages also maintain the patency of the “internal nasal valve,” which is the term for the narrow aperture just inside the nose. The “internal nasal valve” is bordered by the caudal (bottom) edge of the upper lateral cartilage, the nasal septum, and the floor of the nose. Collapse of the internal nasal valve can result in breathing difficulties and may require surgery to correct. When the “internal nasal valve” is collapsed, it can usually be improved with a “spreader graft” placed between the upper lateral cartilage and the septum. Special consideration is allowed for the upper lateral cartilages during rhinoplasty to minimize the alteration of the airway with aesthetic surgery.
The skin anatomy of the nose also plays an important role in the appearance of the nose. There are two factors related to the nasal skin that affect the appearance. The first factor is nasal skin thickness. The thickness of the nasal skin varies widely from patient to patient and can be very thin, or very thick. When the nasal skin is very thick, changes to the nasal skeleton (cartilage and bone) will be less noticeable after rhinoplasty. In other words, it is more difficult to achieve nasal tip definition in the patient with thick nasal skin. This is because the thickness of the nasal skin somewhat conceals the detailed anatomy of the nasal skeleton. The advantage of thick nasal skin is that irregularities and small asymmetries will be less noticeable. The second factor is the amount of subcutaneous fat. When more definition is desired in the patient with thick nasal skin, the nasal tip can be “defatted” during the rhinoplasty. This will increase the tip definition to some degree. Some patients have very thin nasal skin, in which case small irregularities or asymmetries are more likely to be visible. If an irregularity of the nasal skeleton does exist after rhinoplasty, it will become more obvious as the swelling subsides. The advantage of thin nasal skin is that excellent tip definition can be obtained with rhinoplasty. If nasal grafts are needed, thin nasal skin may make the graft borders more visible, so this should be taken into account when designing and placing the graft.
What’s the Difference Between Open & Closed Rhinoplasty?
There are two basic approaches to aesthetic rhinoplasty. One is termed “open rhinoplasty” and the other is termed “closed rhinoplasty.” The “closed rhinoplasty” technique was ubiquitously performed for aesthetic rhinoplasty for many years with good results. The “closed rhinoplasty” technique was preferred at that time to avoid external scars. During this period, it was not specifically referred to as the “closed technique” because there was no other commonly performed “open technique” to compare. With the “closed rhinoplasty” technique, the incisions were made inside the nose, so there was no visible external scar. The disadvantage of this technique was that the procedure was done “blindly” (to some degree), meaning that it was done by “feel” and not sight. Another distinct disadvantage is that complex surgical maneuvers used to shape the nose were impossible due to lack of access and exposure. The “open rhinoplasty” technique was used during this period of time, but was primarily used for congenital defects and trauma patients. Recently, the “open rhinoplasty” technique has gained wide acceptance and is used for routine rhinoplasty procedures.
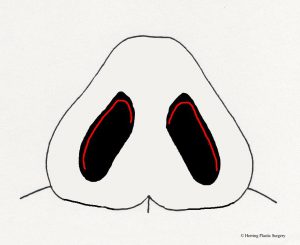
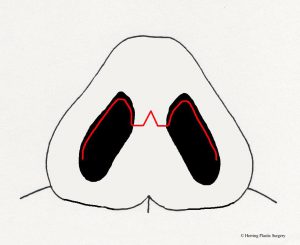
- Incisions for “closed rhinoplasty”
- Incision for “open rhinoplasty”
The “open rhinoplasty” technique has an external incision in the columella (between the nostrils just under the nasal tip). The advantage of the “open rhinoplasty” technique is the ability to perform the rhinoplasty procedure under direct vision, meaning the surgeon can directly see the structures that are being altered. Many surgeons feel that this allows more accuracy and predictability with the rhinoplasty procedure. It also allows more options to alter the nasal skeleton, which gives superior aesthetic results—especially in more challenging cases. One disadvantage of the “open rhinoplasty” procedure is the external visible scar, although the scar will virtually disappear in many patients. Even if the scar does not disappear, its location in the columella makes it very inconspicuous. Many surgeons feel that the advantages of direct vision of nasal structures during the rhinoplasty procedure far outweigh the disadvantage of an external scar. Another perceived disadvantage is temporary prolonged edema (swelling) of the nasal tip. That said, many surgeons feel that the advantages of direct vision of nasal structures during the rhinoplasty procedure far outweigh the temporary swelling that may occur in some patients. As a result, many surgeons that use the “open rhinoplasty” method do not feel that the perceived increased swelling is of any consequence. One final potential problem with the “open rhinoplasty” technique is compromised blood supply to the tissues. This should always be considered when the “open rhinoplasty” approach is chosen.
A key advantage of “open rhinoplasty” is that it allows the plastic surgeon to accurately “de-fat” the nasal tip when this is indicated. In some patients, there is a relatively thick area of fat under the skin of the nasal tip. This ancillary procedure may be used when the patient has thick nasal skin and more definition in the nasal tip is desired. “Defatting” in this context does not mean removal of all the subcutaneous fat. Instead, “defatting” means thinning or reducing the thickness of the fat. Some thickness of fat should be left behind to allow smooth contours and, most importantly, maintain circulation to the nasal tip. If the nasal tip is “defatted” by feel with the “closed rhinoplasty” technique, circulation problems can occur because too much fat was removed. Further, because the “defatting” is imprecisely done by feel, contour irregularities and asymmetry may occur.
As with all plastic surgery procedures, no single technique is best for every patient. There are no hard and fast rules about which technique should be used in which situation. The best technique for a particular patient depends on many factors, some of which are in the table below. The aforementioned are general considerations for choice of technique. The surgeon’s experience level is also a factor in which technique is chosen.
Indications for Choice of Rhinoplasty Technique
Simple nasal tip changes
Simple dorsum changes
Dorsum is symmetrical
Tip is symmetrical
Grafts not needed
No previous surgery
Thick nasal skin
Patient concerns about external scar
No history of trauma
Open technique
Complex nasal tip changes
Complex dorsum changes
Dorsum is asymmetrical
Tip is not symmetrical
Grafts needed
Previous surgery (revision)
Thin nasal skin
No patient concerns about external scar
History of trauma
What Is Involved with the Rhinoplasty Consultation &
Preoperative Planning?
To begin the rhinoplasty consultation, Dr. Herring will listen to your specific nasal concerns and goals for treatment, giving him a sense of what is bothering you about the appearance and/or function of your nose, as well as the particular improvement(s) you wish to attain.
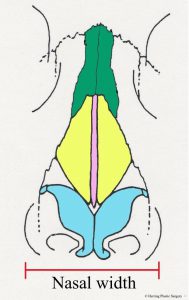
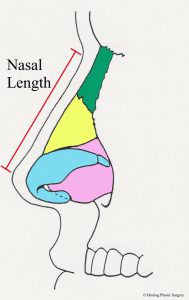
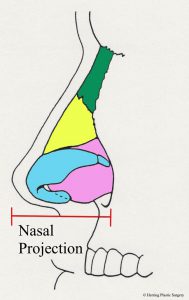
Next, Dr. Herring will evaluate your nose from two general perspectives. The first is to consider the nose as an isolated anatomic entity. General aspects are examined, including shape, size, and angles. The general size of the nose is assessed using three different dimensions. First is the nasal width. This is the largest width of the nose at its base. This dimension is measured as Dr. Herring faces you and is the distance from the base of the outside of one nostril to the outside of the other nostril (see image below). The second and third dimensions are measured from the lateral side (side view). The nasal length is measured from the glabellar area (depression between the eyes) to the nasal tip (see image below). The nasal projection is measured from the base of the nose to the nasal tip (see image below). Any of these dimensions that are outside the normal range can be corrected with rhinoplasty.
- Nasal width
- Nasal length
- Nasal projection
The second general perspective evaluated is nasal shape. The nasal tip may be too narrow, too broad, have too little projection, or have too much projection. The nasal tip may have too much droop or too much elevation. The nasal dorsum may be too wide, too narrow, have a prominent hump, or a concavity. The nose may also be asymmetrical in the dorsum (top, deviated septum) or may have misshapen alar cartilages (the lower part of the nose). All of these non-ideal anatomical situations can be seen in isolation, or in combination. Note that a non-ideal anatomical situation may be seen in both the size and shape evaluations of the nose. For example, if you have a drooping nasal tip seen in the shape evaluation, the nasal length will likely be outside the normal range seen in the nasal length evaluation.
There are many variations of facial shapes that should be considered when planning the rhinoplasty. As noted above, the nose should “match” the facial shape as much as possible after the rhinoplasty procedure. There are as many as nine defined facial shapes termed Kite, Heart, Rectangle, Oval, Round, Square, Teardrop, Heptagon, and Oblong—with the first four being the most common. The “ideal facial shape” has been defined by a number of objective parameters, including the “Golden ratio,” which is the length-to-width ratio of the face (ideal being defined as 1.6 times longer than it is wide). Because there are so many different facial shapes, it follows that there will be many different nasal shapes that will “match.”
There are many other factors to consider when planning a rhinoplasty. Ethnicity also plays a role in the preoperative planning. When considering ethnicity, many plastic surgeons feel that it is inappropriate to erase ethnic characteristics completely. As noted above, proportion and “match” are also very important when considering facial shape, and the same holds for ethnicity. This means that when the so-called “ethnic rhinoplasty” is performed, a good measure of common sense should be applied to help ensure a good overall “match.”
Your gender is also very important when planning a rhinoplasty. There are characteristics that are more frequently identified as masculine, and others that are more frequently identified as feminine. Years ago there were limited maneuvers used in the rhinoplasty procedure, so every patient got the same rhinoplasty. This meant that the 250-pound football player got the same nose as the 90-pound ballerina. With a multitude of rhinoplasty techniques currently available, and a focus on individuality, a bias towards femininity or masculinity can be achieved.
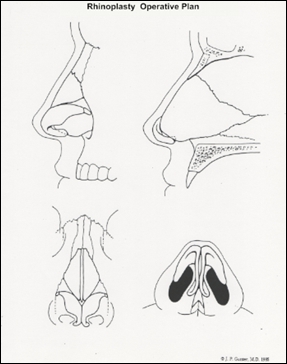
Once all factors have been considered and your goals are completely understood, Dr. Herring will formulate a personalized surgical rhinoplasty plan. Dr. Jack Gunter, a skilled and innovative rhinoplasty surgeon designed a rhinoplasty diagram (below) to plan, record, and explain the plan to patients. This diagram is very helpful and may be used by Dr. Herring (copyright and courtesy of Dr. Jack Gunter) to show you exactly what will be done.
The nose is also assessed in relation to the face. Facial shape as it relates to the nose is a very important aspect of the assessment. There are many variations of nasal shape that still appear to be in perfect proportion because the nose “matches” the face. A “thin” nose may appear normal and in proportion if “matched” with a thin face. A more rounded, bulbous nose may appear perfectly normal and in proportion if “matched” with a round or full face. While there is the concept of an “ideal nose,” this does not mean anything outside that ideal is not attractive. Proportion, in part, defines beauty—and there are many different shapes that can be considered “ideal” if they are in proportion with the face. A good example of this concept is the comparison of two very attractive women with very different noses. Meryl Streep has a thin, less full face and also has a thin nose, which is a perfect match. Dyan Cannon has a more rounded, full face and also has a more rounded nose, which is also a perfect match. The fact that these two women have very different nasal shapes but are both very attractive emphasizes the concept of proportion. Conversely, if the noses of these two actresses were photographically transposed, there would not be a good “match.”
When planning an aesthetic rhinoplasty, it is important to note that the physiologic (functional) aspects of the nose are also considered by Dr. Herring. If the nasal airway is blocked, the etiology is assessed. When the nasal airway is blocked, it is usually the result of a deviated septum or overgrowth of the turbinate bones (scroll shaped bones inside the nose). In many circumstances, the nasal obstruction is corrected at the same time as the aesthetic rhinoplasty.
Throughout the entire planning process, Dr. Herring encourages you to ask any and all questions, and he will never pressure you into anything that makes you uncomfortable. He wants this to be a time of education, allowing you to obtain all the information you need to make an informed decision about your care. In the end, your approval is necessary for Dr. Herring to move forward with surgery.
“Dr. Herring is very knowledgeable in his recommendations for procedures. He is kind and attentive. His staff is sweet. My results exceeded any expectations I had.”
How Is the Rhinoplasty Procedure Performed?
The rhinoplasty procedure has been refined significantly over the past decades. Years ago, the typical rhinoplasty consisted of some very basic surgical maneuvers to change the shape of the nose. Today, the anatomy of the nose has been further studied and defined, and many more surgical maneuvers have been described to refine the final result of the rhinoplasty procedure.
The specific plan for each rhinoplasty is formulated prior to surgery, as detailed in the section above. While there may be small alterations in the surgical plan, the specifics of the plan are understood, set, and approved by you—the patient—before the operation begins.
The two general characteristics that are most commonly altered during the rhinoplasty procedure are the nasal tip and the nasal dorsum. The nasal tip correction consists of alterations of the cartilages at the bottom of the nose—the alar (lower lateral) cartilages and the cartilaginous septum (cartilage plate in the bottom of the midline of the nose). Many different maneuvers are used to change the shape, size, and position of these cartilages to achieve the desired aesthetic result, and several of the more complex maneuvers are more easily and accurately performed with the “open rhinoplasty” technique.
Changes to the nasal dorsum—such as raising, lowering, or straightening—can be made under direct vision with the “open rhinoplasty” technique, or they can be made without direct vision using the “closed rhinoplasty” technique. In some circumstances, a graft is needed on the nasal dorsum to correct the contour deformity.
Rhinoplasty can be performed on most patients with local anesthesia and intravenous sedation. The length of time of the rhinoplasty procedure varies widely depending upon the complexity of the surgery. For example, if the nasal tip is the only part of the nose that will be changed, then the operation will last about an hour or less, on average. If the entire nose is changed and there are breathing problems that also need to be addressed, then the operation would take longer to complete. The rhinoplasty surgery is an outpatient procedure for most patients, which means that you will likely be able to go home after the surgery.
For more detailed information about the specific surgical maneuvers used during rhinoplasty, please visit our page devoted to rhinoplasty techniques.
What Is Recovery from Rhinoplasty Like?
Recovery following rhinoplasty is usually quite rapid. There is some swelling after surgery, but a significant percentage will resolve in the first two weeks. In some patients, there is also some bruising (ecchymosis)—though this also typically subsides in about two weeks. The amount of bruising depends in part on the surgery that is needed, and the more extensive the surgery, the more bruising that can be expected.
Most of the sutures used in the rhinoplasty procedure are absorbable (they will not have to be removed by Dr. Herring). There are typically a few external sutures used for the “open rhinoplasty” technique that are removed about five days after surgery. In years past, a splint was used (plaster) after rhinoplasty, but some studies showed that the splint was not beneficial, so Dr. Herring does not typically use this protocol any longer.
In some circumstances, there is extra swelling (edema) in the nasal tip, and this is sometimes improved with a weak steroid injection. If bandages are placed, they are also removed in about five days.
In the first week after the rhinoplasty, it is helpful to elevate the head, which not only aids in limiting the amount of swelling, but also helps more quickly resolve the swelling that does occur. Daily living activities can be performed the day after surgery by most patients. Returning to work after rhinoplasty surgery will depend on a number of factors, including the type of rhinoplasty required, the type of job, the particular work environment, and the wishes of the patient. Most individuals that work with the public are able to return in about one week.
Throughout the recovery process, it is important that you exercise caution to prevent any nasal trauma after rhinoplasty. The delicate structures of the nose can be easily displaced after rhinoplasty even with minor trauma. You should not place yourself in any situation that increases the risk of nasal trauma (soccer, softball, martial arts, basketball) for at least six weeks.
Regarding follow-up care, you will likely be seen by Dr. Herring on a weekly basis for about one month after surgery. Subsequently, appointments are spaced further apart on a three to six month basis. The soft (cartilage, skin, fat) and hard tissues (bone) remodel for up to two years after rhinoplasty, so it is important that Dr. Herring follows you during this time frame. If small revisions are needed after rhinoplasty, they will generally be done after the two year healing period.
How Much Does Rhinoplasty Cost?
The cost of rhinoplasty at Herring Plastic Surgery usually starts at $7,200, which includes Dr. Herring’s surgeon fee, all surgical facility expenses, anesthesia charges, and prescription medicines. Dr. Herring is able to offer rhinoplasty at such a competitive rate due to our onsite, accredited surgery facility, which enables him to perform the procedure in a center that meets all of the same safety standards as a hospital—without the associated fees. Patients also benefit from the improved convenience and heightened privacy of our state-of-the-art center.
For personalized rhinoplasty pricing, you will need to schedule a consultation with Dr. Herring. At this time, he can provide a quote based on your specific needs and goals for treatment. If desired, a member of our team can also introduce you to numerous plastic surgery financing options that can help make rhinoplasty affordable for almost any budget.
Additional Frequently Asked Questions About Rhinoplasty
What is the history of rhinoplasty?
There is a very long and rich history regarding the nose and rhinoplasty. The nose has been the focus of writers, philosophers, and physicians for many centuries. Gasparo Tagliacozzi (1545–1599) developed the “Italian method” of nasal reconstruction, and his description of this method is thought to be the first practical treatise in the specialty of plastic surgery. The well-known play, Cyrano De Bergerac, written by Edmund Rostand in 1897, describes a man with self-doubt due to his very large nose. The Adventures of Pinocchio, written by Carlo Lorenzini in 1880, is a novel about a marionette whose nose grew longer when he told lies. So ingrained into modern culture is this novel, that pundits assign a “Pinocchio count” (four Pinocchios being the worst) for perceived dishonesty in the media. These are just a few of the many well-known examples of the nose being the center of literature and medicine in years past.
Rhinoplasty has become one of the most popular procedures in aesthetic plastic surgery. Modern day rhinoplasty can be partly credited to Dr. Jacques Joseph (1865–1934), and while these techniques are considered crude by today’s standards, his work brought attention to this very specialized area of plastic surgery, which led to focused research on the topic. The Joseph procedure was described over a century ago and was arguably the beginning of the modern era of rhinoplasty. While Dr. John Roe (1848–1915) was thought to be the first to perform the intranasal rhinoplasty, more credit is given to Joseph because he popularized the rhinoplasty procedure. Dr. Roe’s scientific paper on rhinoplasty was published in 1887. As a result of plastic surgery research and improvements in instrumentation, the basic rhinoplasty has improved dramatically in the last three-plus decades.
The most significant change in the technical aspect of cosmetic rhinoplasty is the concept and principle of conservatism. Conservatism in this context means limited change with the rhinoplasty procedure. Early cosmetic rhinoplasty procedures, and even rhinoplasty procedures for functional problems, were characterized by unnecessary excessive removal of nasal tissues (cartilage and bone). This procedure is now referred to with negative connotations as a “reduction rhinoplasty.” In modern cosmetic rhinoplasty, what the plastic surgeon leaves in the nose is just as important as what the surgeon removes from the nose, and is arguably more important. Stevie Ray Vaughn, the legendary electric blues guitarist, underwent a reduction rhinoplasty at age six around 1960. This has been written about extensively in his biographies, and those books imply that he was left with very little cartilaginous nasal septum following this surgery. Images of him later in life reveal a depressed nasal dorsum, sometimes referred to as a “saddle nose.” While the reduction rhinoplasty may have been the standard of care in 1960, it is not the standard today.
The nose can be thought of as having the same “design principles” as a camping tent. A camping tent is supported by a frame (“internal skeleton”) constructed of wood, plastic, or metal, and the frame is what gives the tent its shape. Once the tent frame is assembled, a covering is draped over the frame, and the covering takes the shape of the frame. The frame is what determines the tents shape and size. If the shape of the frame is changed, then the shape of the tent covering changes. The anatomy of the nose works in a similar manner. The frame (“internal skeleton”) consists of cartilage and bone. The cartilage and bone provide the internal support for the nose. The cartilage and bone would be analogous to the wood, plastic, or metal frame of the tent. The skin of the nose would be analogous to the tent covering. The skin of the nose drapes over the cartilage and bone just as the tent covering drapes over the frame of the tent. In order to change the size and shape of the nose, the internal skeleton (cartilage and bone) is changed. As the internal skeleton of the nose changes, the skin re-drapes over the new supportive shape. Because the nasal skin is elastic, it naturally re-drapes over the newly shaped internal nasal skeleton after rhinoplasty. As a result, there is no need to remove “extra skin” during the rhinoplasty procedure.
If the correct anatomical support of the nose (cartilage and bone) is not preserved during the rhinoplasty procedure, the nose becomes an amorphous blob without defined shape. If the correct anatomical support of the nose is not preserved, then sub-optimal aesthetic issues can result. The nose can lose tip projection so that it appears too small. One can lose dorsal support as in the case of Stevie Ray Vaughn, which can result in a “saddle nose.” This can be particularly pronounced when scar contracture pulls the nasal skin during healing and there are no supporting structures to resist that force. From a functional standpoint, loss of support can also result in airway obstruction. When these situations occur, the repair procedure then falls into the reconstructive realm. This procedure is called a secondary (or revision) rhinoplasty, and this procedure is typically much more challenging than a primary (first) rhinoplasty. Preservation of adequate nasal skeletal support during rhinoplasty is critical, which has led to the accepted concept of conservatism. The conservative rhinoplasty is in stark contrast to the reduction rhinoplasty, where no thought or effort was made to preserve critical anatomic nasal skeletal structures, thereby preserving shape and function. It is the concept of conservatism that has ushered in the modern rhinoplasty.
As an example of how the current “standards” of plastic surgery have changed, one can consider the evolution of the surgical maneuvers used to resize and re-shape the alar (lower lateral) cartilage. The previously noted Joseph procedure frequently transected (divided) the alar cartilages in attempting to improve the nasal tip. This maneuver (reportedly) frequently resulted in kinking of the nasal tip, asymmetry, and an overall unfavorable outcome. The records (images) of the results of the Joseph rhinoplasty are less than detailed because the science of photography was in its infancy at the time. Because nasal aesthetics are a direct reflection of the nasal skeleton, any irregularities or asymmetries in the nasal skeleton are observable after surgery. This is particularly true in patients with thin nasal skin. As a result of the less than optimal results with the Joseph procedure, years later plastic surgeons were taught to never transect the alar. For a period of time, transecting the alar was considered taboo by many plastic surgeons.
Other surgical maneuvers were adopted in lieu of alar transection in an attempt to attain the desired shape of the nasal tip, such as cartilage “scoring.” This technique takes advantage of the natural tendency of cartilage to curve when “scored,” but this procedure has somewhat unpredictable results. The result of the “scoring technique” in some patients was a somewhat bulbous amorphous nasal tip, which was not ideal, but was certainly superior to the Joseph procedure. The unpredictable results with the “scoring technique” led some plastic surgeons to re-examine the alar cartilage transection technique. The new interest in the “open rhinoplasty” technique led to the “rediscovery” of the alar cartilage transection technique. After the “rediscovery” of the alar cartilage transection technique, surgeons realized that with meticulous surgical technique, and a more thorough understanding of the nasal anatomy, the alar cartilage could be transected safely and effectively to achieve the anatomically ideal nasal tip anatomy. The alar cartilage transection maneuver, when properly performed, has resulted in a predictable, well-defined, anatomically ideal nasal tip. Further, the nasal tip can be “customized” to match a patient’s facial shape as well as other individual factors. Transection of the alar cartilages is now commonly performed during rhinoplasty with excellent aesthetic and physiological results. With the latest techniques, the problems with the Joseph procedure were completely eliminated. In summary, the surgical maneuvers to improve the aesthetics of the alar cartilage during rhinoplasty went full circle in about one hundred years.
Another example of the evolution of “standards” of plastic surgery is the approach to rhinoplasty. In Dr. Joseph’s original technique, he used an “open rhinoplasty” technique. This technique used external incisions (as opposed to incisions made inside the nose), which allowed direct vision of the nasal anatomy. This is a great technical advantage for the surgeon. The “open rhinoplasty” technique allows precise surgical alterations of the nasal anatomy to achieve a very predictable aesthetic result. This technique is also very safe. The ostensible disadvantage of the “open rhinoplasty technique” is the visible scars that result. The “open rhinoplasty” technique for aesthetic rhinoplasty fell into disfavor for a long period of time, during which time the “closed rhinoplasty” technique (which involves incisions made inside the nose) was used. Also called the “endonasal approach,” the “closed rhinoplasty” technique did not have external scars but did have the significant disadvantage of not directly visualizing the nasal structures during the procedure. In other words, the procedure was performed “blindly,” meaning by “feel” and not under direct vision. As a result, the “closed rhinoplasty” method is less accurate and less predictable in some circumstances, and especially in the more complicated rhinoplasty procedures. Further, there are many maneuvers that can be utilized during the “open rhinoplasty” procedure that are difficult or impossible with the “closed rhinoplasty” technique. As a result, aesthetic results with the “closed rhinoplasty” approach were inferior to the “open rhinoplasty” technique in some patients. The minimal external scars which were previously a concern with the “open rhinoplasty” technique are now considered (and are) inconsequential. The minimal external scar from the “open rhinoplasty” technique, which is measured in millimeters and is in an inconspicuous area of the nose, virtually disappears with time. About 100 years after Dr. Joseph described his rhinoplasty technique, the “open rhinoplasty” method has regained great popularity and is now widely used.
Modern rhinoplasty techniques are very safe and very predictable. In a properly screened patient population, the satisfaction rate is very high. Most patients that undergo a cosmetic rhinoplasty state that they would make the same decision again to get the surgery if privileged with that opportunity.
Can breathing problems be corrected at the same time as aesthetic rhinoplasty?
Yes. Breathing problems can typically be corrected at the same time as aesthetic rhinoplasty. While aesthetic rhinoplasty is generally considered an elective surgery, if breathing problems are present, it is usually considered a medically necessary procedure.
What is meant by “realistic expectations” for rhinoplasty?
Realistic expectations means that rhinoplasty can change the shape of the nose—not that your nose will look exactly like anybody else’s nose, including your family members. It also does not mean any other problems will be solved by getting rhinoplasty. Rhinoplasty simply changes the appearance of the nose you were born with.
What type of anesthesia is used for rhinoplasty?
Anesthesia for rhinoplasty is different from many other types of anesthesia techniques. Like anesthesia for other plastic surgery procedures, the area of surgery should be without sensation for the duration of the surgery. Unlike anesthesia for many other plastic surgery procedures, the desired changes in the nose are so small in most patients, that any distortion of the tissue from anesthesia will make the procedure more difficult. As such, the goal for anesthesia with the rhinoplasty procedure is to obtain a block of the sensation while at the same time avoiding distortion of the tissues of the nose.
Anesthesia for rhinoplasty is somewhat unique because it is delivered by anesthesia professionals and plastic surgeons. The anesthesia professional provides the intravenous medication and the plastic surgeon provides the local anesthesia. In other words, anesthesia for the rhinoplasty procedure is a team approach. For most patients, a combination of intravenous sedation and local anesthesia (similar to that used by dentists) works well. Because the intravenous sedation is administered to the patient before the local anesthesia, the patient will experience no discomfort when it is given. The local anesthesia technique that can be used for rhinoplasty surgery is termed a field block. With this type of local anesthesia, the nerves to the nose are blocked outside the area of surgery so that the tissues are not distorted. While there may be some tissue distortion from the surgery itself, by using a field block, the general anatomy of the nose can be observed during the procedure. As a result, the final aesthetic result becomes much more predictable.
Because the neuroanatomy of the nose is very complex (many different sensory nerves innervate the nose), multiple injections of local anesthetic are required. This emphasizes the importance of a thorough knowledge of the sensory nerves of the nose, which facilitates a complete anesthetic block. In addition to local anesthesia injections, topical anesthesia can also be used. Topical anesthesia means that the drug is absorbed into tissues rather than being injected.
In addition to blocking sensation to the nose, in most circumstances, a local anesthetic solution with epinephrine is used. Epinephrine is a natural vasoconstrictor (causes blood vessels to become smaller). As a result, there is less bleeding into the surgical field, making structures more visible. Operating in a “bloodless field” is a basic principle of surgery that is very important during the rhinoplasty procedure.
Modern anesthesia medicines (intravenous medicine) have a very short half-life (go away quickly), have a low allergic potential (very few allergic problems), have a broad dosage curve, and are ideal for surgical procedures of this length. The short half-life of the drugs allow the patient to wake up quickly, which is ideal for outpatient surgery. The low allergic potential means that the drugs are generally very safe from this standpoint. The broad dosage curve allows the anesthesia staff to reach the precise depth of sedation required.
In summary, modern anesthetic techniques used by qualified anesthesia professionals during rhinoplasty make the patient very comfortable and are considered very safe.
In some circumstances, general anesthesia may be required if there are concerns about compromise of the patient’s airway. This circumstance may arise when extensive intra-nasal surgery is required, such as septal repair and/or excision of the inferior turbinate bones to treat breathing problems.
What surgical instruments are used to perform rhinoplasty?
The rhinoplasty procedure is performed with a very specialized set of instruments designed specifically for that purpose. These instruments have been improved and refined over the years, which has made the procedure much easier. The specialized instruments for rhinoplasty fall into three categories. The first category assists in gaining access to the nasal structures. This allows specific surgical maneuvers to be performed with accuracy. Included in this group of instruments are specialized scissors and other instruments used for freeing the tissues. The second group of instruments assist in providing exposure of the nasal structures to facilitate the rhinoplasty procedure. This group of instruments includes specialized types of retractors designed specifically for rhinoplasty. The last group of instruments are those that alter the tissues. This group of instruments includes specialized scissors, rasps, and osteotomes (bone instruments). The instruments for rhinoplasty have specialized shapes and sizes and are used (almost) exclusively for this procedure.
Will I have swelling or bruising after rhinoplasty?
The amount of swelling and bruising after rhinoplasty varies from patient to patient. There is always some swelling after any surgical procedure, including rhinoplasty. In some patients, there is severe bruising after surgery, and in others there is no bruising. If there is bruising after rhinoplasty, it will usually go away in about one to two weeks. The swelling after rhinoplasty goes away gradually, most of it going away after several weeks. The final part of the swelling takes longer to resolve, and that is why the final shape of the nose is not seen immediately after the procedure.
Does rhinoplasty hurt?
In most patients, there is very little discomfort after rhinoplasty. Patients have a sensation of “stuffiness” following treatment, which usually goes away after one week. The amount of discomfort is also related to how much surgery is done during the rhinoplasty procedure, which varies from patient to patient.
When can I go back to work after rhinoplasty?
In most cases, it is possible to go back to work a few days after surgery. However, because rhinoplasty is obvious immediately after surgery, some patients will take about one week off so that most of the bruising and some of the swelling has gone away. If the work involves extreme exertion, then some patients will stay out of work longer than one week. As with any surgery, including rhinoplasty, if you are taking strong pain medicine, it is important not to drive while taking that medicine.
When can I drive after rhinoplasty?
Most patients are able to drive a couple of days after rhinoplasty, as long as they are not taking prescription-strength pain medicine.
Where can I get more information about rhinoplasty?
Information on rhinoplasty is widely available from many sources, though the best place to get information is from a board-certified plastic surgeon trained to diagnose the cause of nasal appearance concerns, and further, to correct those problems with surgical techniques. Most importantly, the plastic surgeon can explain what can be changed with nose reshaping and the specific techniques that are appropriate for your specific situation.
Book a Rhinoplasty Consultation with Dr. Herring
To learn more about rhinoplasty, or if you are interested in treatment and wish to schedule a consultation with Dr. Herring, please contact our practice online or by telephone today.